Mental Health 3.0: Why Investors Are Betting on Navigation, Not Just Meditation
Mental health has long been a high-growth vertical in digital health, but the landscape is shifting once again. In a market once dominated by on-demand therapy and meditation apps, we’re now seeing growing investor enthusiasm for startups that navigate care, integrate across the system, and close the loop on outcomes. Welcome to Mental Health 3.0 — where navigation is the killer app.
The global mental health tech market is projected to reach $66 billion by 2032, with a CAGR of 15.6%, but more importantly, it’s evolving. As mental health becomes a systemic challenge — not just a consumer one — startups are rethinking product, service, and payment models to reflect the complexity of care. And VCs are taking notice.
Why It’s Happening: The Shift from Point Solutions to Ecosystems
During the pandemic, the first major wave of mental health investment went toward single-point solutions — from therapy platforms like BetterHelp to mindfulness apps like Calm. But even as usage spiked, many of these companies struggled with engagement, retention, and reimbursement.
Now, with the rise of value-based care and broader shifts in healthcare delivery, a new generation of startups is emerging — focused on care coordination, navigation, and integration with primary care, employers, and payers.
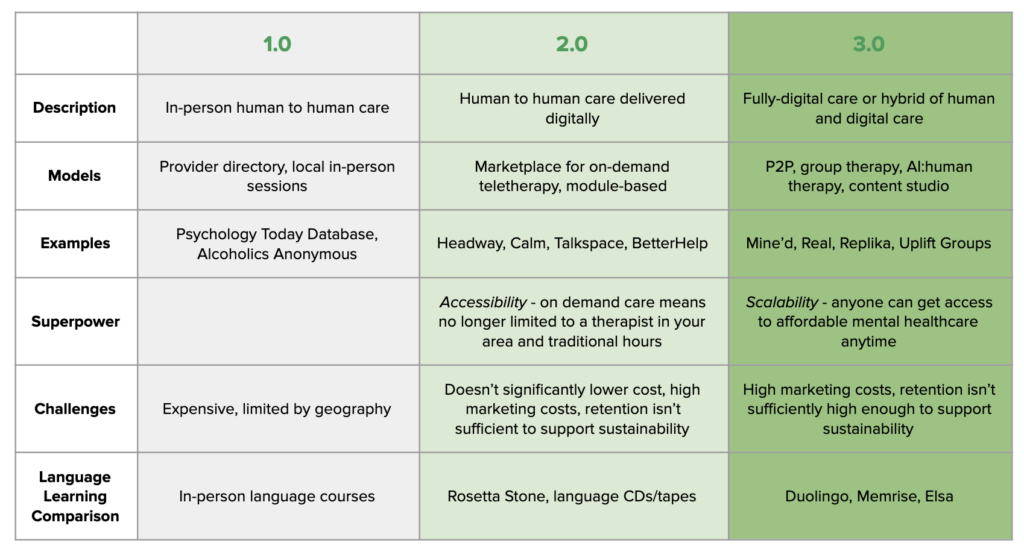
Illustration by Union Square Ventures
Who’s Making Noise?
Solace: Raised a $60M Series B in March 2025. The company offers tech-enabled care navigation for mental health patients, with a focus on the Medicare population. By combining human advocates, digital tools, and system integration, Solace helps patients find, afford, and stay with the right care.
Violet: A cultural competence platform that partners with health plans and mental health providers to match diverse patients with inclusive clinicians, improving access and outcomes for underserved populations.
Spring Health: Now a scale-stage company, Spring continues to innovate beyond therapy by integrating with employee benefits platforms and adding predictive analytics to help HR teams intervene earlier.
What’s Coming Next: Reimbursement, AI, and Outcomes-Based Models
As CMS and commercial payers expand reimbursement for behavioral health integration and care management, startups in this space are well-positioned to thrive. We’re also seeing:
- AI-powered care triage tools that direct patients to the right level of care faster
- Patient-reported outcomes (PROs) becoming the norm in employer contracts
- More hybrid models combining tech and human care — particularly in senior care and Medicaid
Mental health tech is no longer just about scale — it’s about impact and integration. Investors are betting on startups that can fit into the broader healthcare puzzle, demonstrate ROI, and build sticky infrastructure. While the early wave of consumer-facing mental health tools laid the groundwork, it’s this third wave — focused on navigation, outcomes, and collaboration — that’s drawing serious capital.
—————————————–
If you are a builder, investor or researcher in the space and would like to have a chat – please reach out to me at amit.k@thelotuscapital.com